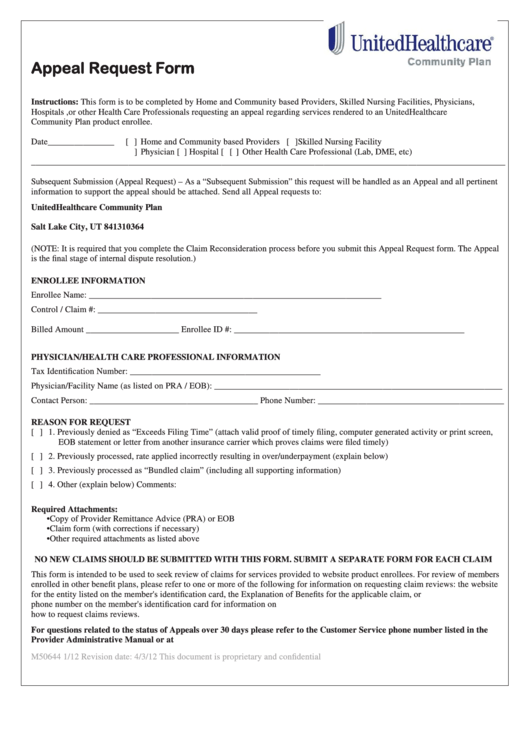
United Health Care Provider Appeal Form - Appeal requests must be submitted in writing and should clearly state “formal appeal request.” providers should state the specific reason for. Incomplete submissions will be returned. Complete all information required on the “request for claim review form”. To file an appeal in writing, please complete the medicare plan appeal and grievance form (pdf) (760.99 kb) and follow the instructions. To request reconsideration, health care professionals have 180 days from the date a claim is denied in whole or partially. The unitedhealthcare provider portal allows you to submit referrals, prior authorizations, claims, claim reconsideration and appeals,.
The unitedhealthcare provider portal allows you to submit referrals, prior authorizations, claims, claim reconsideration and appeals,. Appeal requests must be submitted in writing and should clearly state “formal appeal request.” providers should state the specific reason for. To request reconsideration, health care professionals have 180 days from the date a claim is denied in whole or partially. Complete all information required on the “request for claim review form”. Incomplete submissions will be returned. To file an appeal in writing, please complete the medicare plan appeal and grievance form (pdf) (760.99 kb) and follow the instructions.
The unitedhealthcare provider portal allows you to submit referrals, prior authorizations, claims, claim reconsideration and appeals,. Incomplete submissions will be returned. To file an appeal in writing, please complete the medicare plan appeal and grievance form (pdf) (760.99 kb) and follow the instructions. Appeal requests must be submitted in writing and should clearly state “formal appeal request.” providers should state the specific reason for. Complete all information required on the “request for claim review form”. To request reconsideration, health care professionals have 180 days from the date a claim is denied in whole or partially.
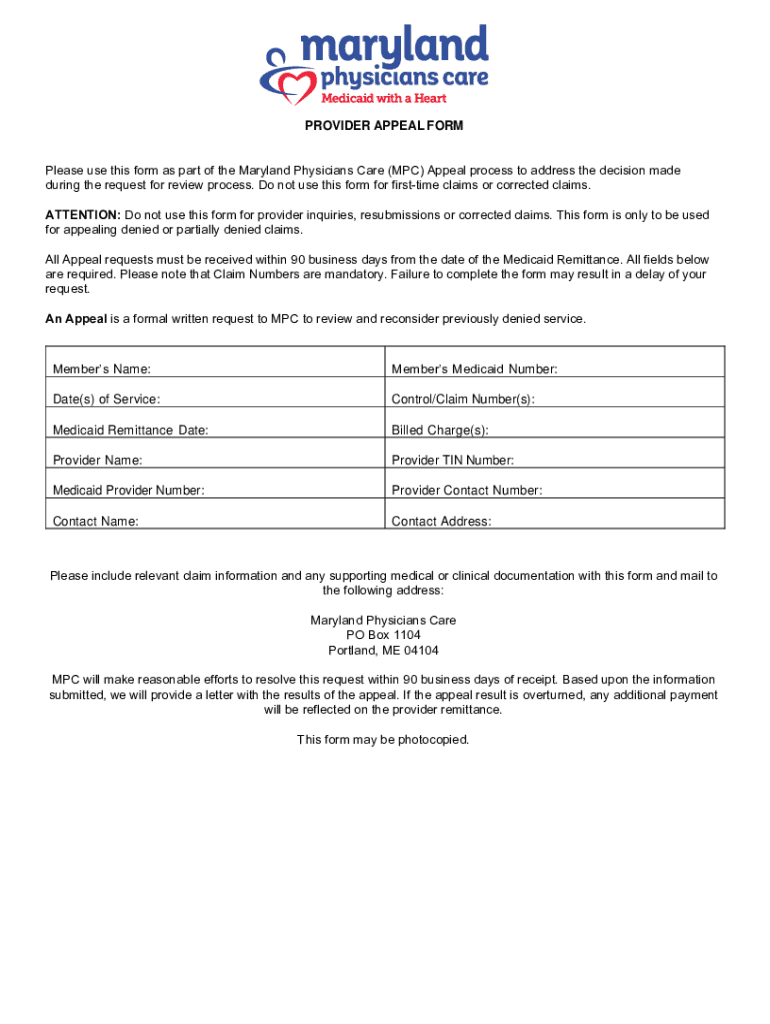
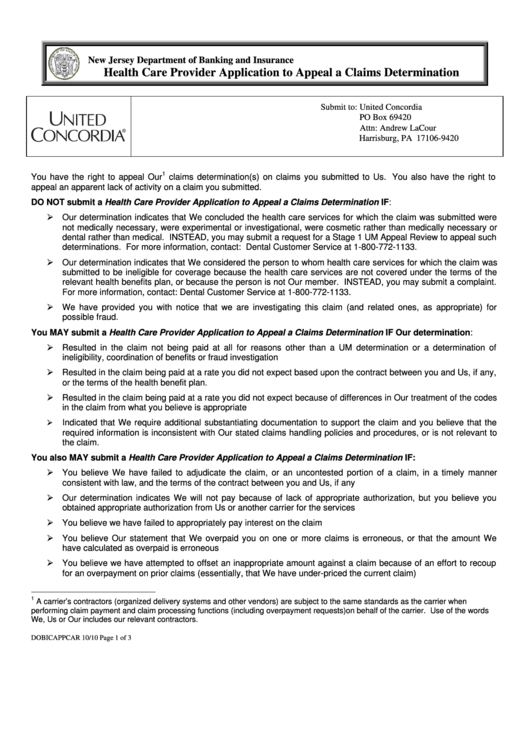
Fillable Online Maryland Physicians Care Provider Appeal
The unitedhealthcare provider portal allows you to submit referrals, prior authorizations, claims, claim reconsideration and appeals,. Incomplete submissions will be returned. Appeal requests must be submitted in writing and should clearly state “formal appeal request.” providers should state the specific reason for. Complete all information required on the “request for claim review form”. To request reconsideration, health care professionals have.
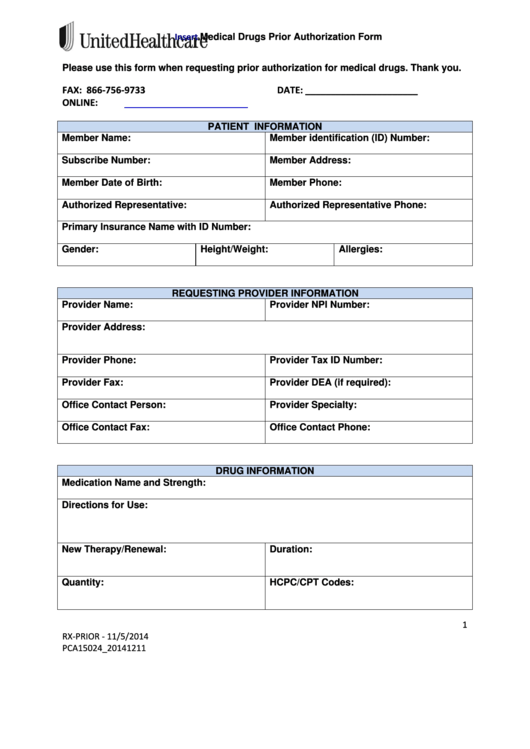
Top 16 United Healthcare Prior Authorization Form Templates free to
The unitedhealthcare provider portal allows you to submit referrals, prior authorizations, claims, claim reconsideration and appeals,. To request reconsideration, health care professionals have 180 days from the date a claim is denied in whole or partially. To file an appeal in writing, please complete the medicare plan appeal and grievance form (pdf) (760.99 kb) and follow the instructions. Incomplete submissions.
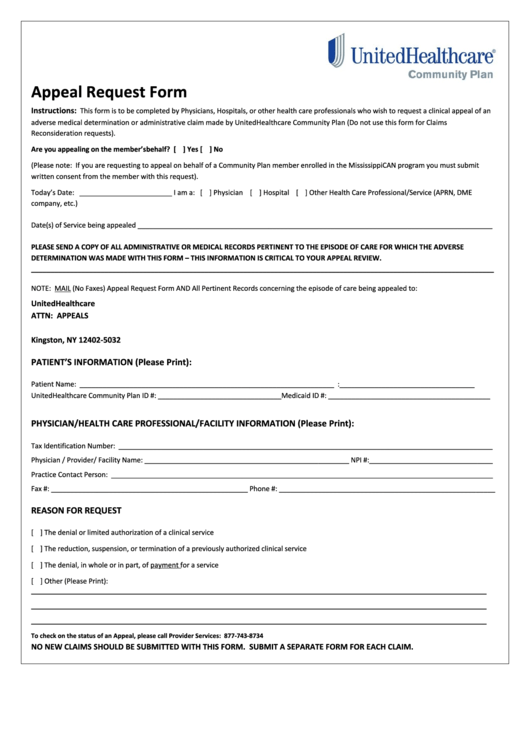
Fillable Online Physician/Provider Appeal Request Form Fax Email Print
Complete all information required on the “request for claim review form”. The unitedhealthcare provider portal allows you to submit referrals, prior authorizations, claims, claim reconsideration and appeals,. To request reconsideration, health care professionals have 180 days from the date a claim is denied in whole or partially. Incomplete submissions will be returned. To file an appeal in writing, please complete.
United Health Care Community Plan Forms
To request reconsideration, health care professionals have 180 days from the date a claim is denied in whole or partially. The unitedhealthcare provider portal allows you to submit referrals, prior authorizations, claims, claim reconsideration and appeals,. Incomplete submissions will be returned. Appeal requests must be submitted in writing and should clearly state “formal appeal request.” providers should state the specific.
Medicare Appeal Form Cms20027 Medicare (United States) Medicaid
Incomplete submissions will be returned. The unitedhealthcare provider portal allows you to submit referrals, prior authorizations, claims, claim reconsideration and appeals,. To file an appeal in writing, please complete the medicare plan appeal and grievance form (pdf) (760.99 kb) and follow the instructions. Complete all information required on the “request for claim review form”. To request reconsideration, health care professionals.
Alignment Health Plan Provider Appeal Form
Complete all information required on the “request for claim review form”. To request reconsideration, health care professionals have 180 days from the date a claim is denied in whole or partially. The unitedhealthcare provider portal allows you to submit referrals, prior authorizations, claims, claim reconsideration and appeals,. Appeal requests must be submitted in writing and should clearly state “formal appeal.
Top United Healthcare Appeal Form Templates free to download in PDF format
Incomplete submissions will be returned. Complete all information required on the “request for claim review form”. To file an appeal in writing, please complete the medicare plan appeal and grievance form (pdf) (760.99 kb) and follow the instructions. Appeal requests must be submitted in writing and should clearly state “formal appeal request.” providers should state the specific reason for. To.
56 Top Images United Healthcare Appeal Form Https Www Wellcare Com
To request reconsideration, health care professionals have 180 days from the date a claim is denied in whole or partially. Appeal requests must be submitted in writing and should clearly state “formal appeal request.” providers should state the specific reason for. Incomplete submissions will be returned. The unitedhealthcare provider portal allows you to submit referrals, prior authorizations, claims, claim reconsideration.
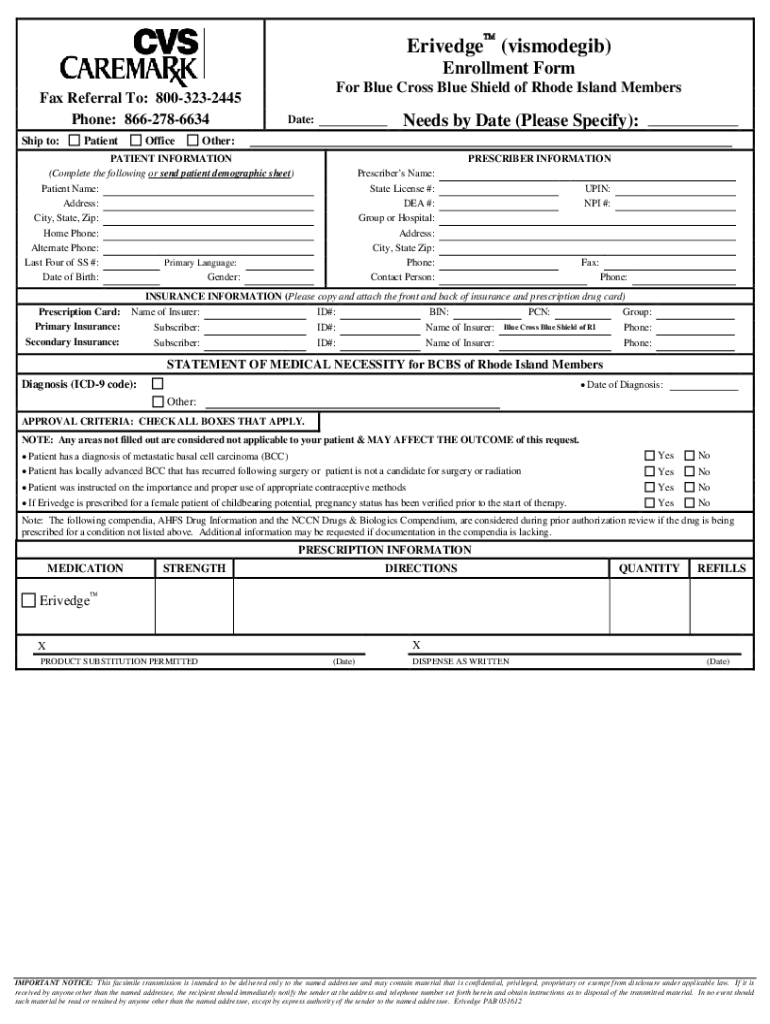
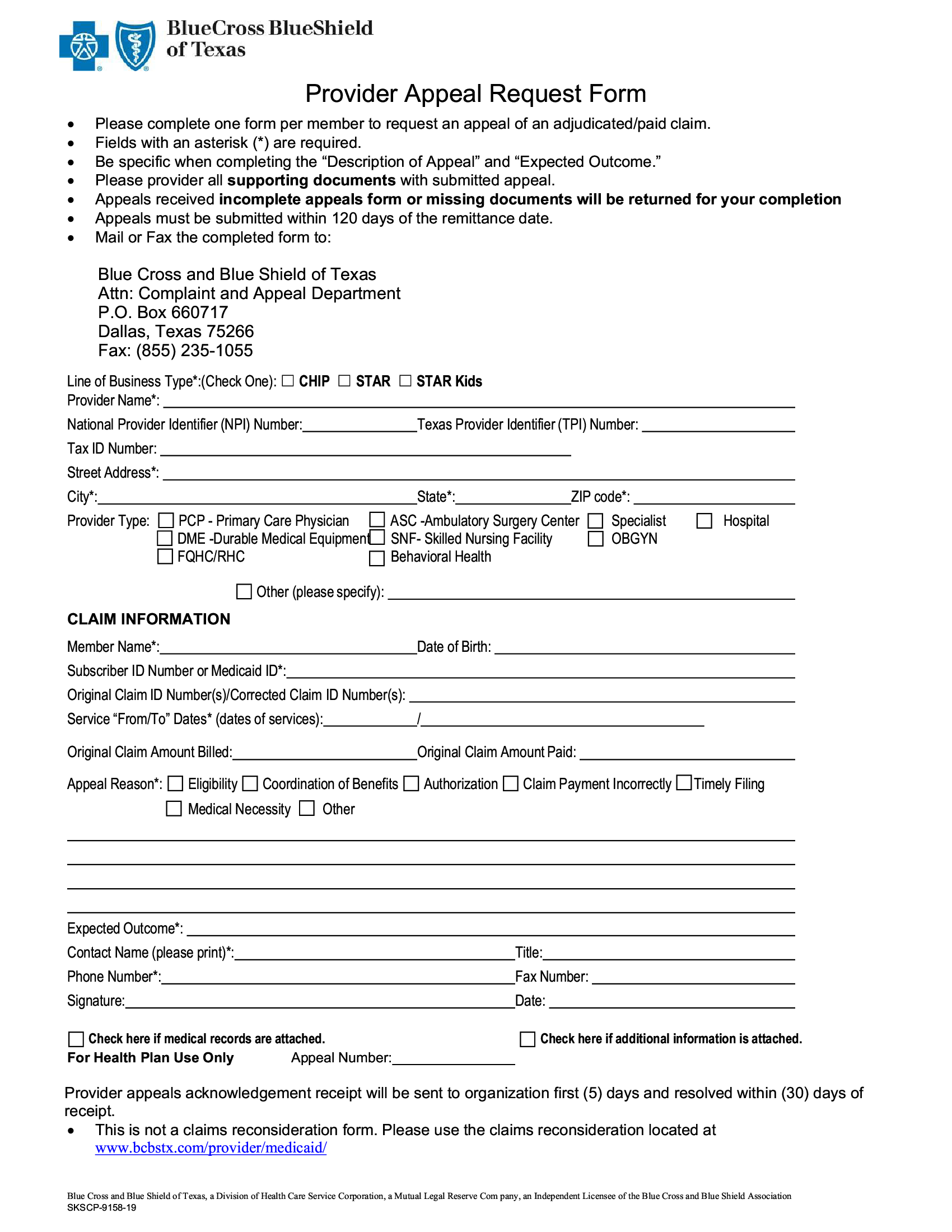
BCBS Provider Appeal Request Form Forms Docs 2023
Incomplete submissions will be returned. Complete all information required on the “request for claim review form”. To request reconsideration, health care professionals have 180 days from the date a claim is denied in whole or partially. Appeal requests must be submitted in writing and should clearly state “formal appeal request.” providers should state the specific reason for. The unitedhealthcare provider.
United Healthcare Insurance Appeal Form Financial Report
The unitedhealthcare provider portal allows you to submit referrals, prior authorizations, claims, claim reconsideration and appeals,. To request reconsideration, health care professionals have 180 days from the date a claim is denied in whole or partially. Incomplete submissions will be returned. Appeal requests must be submitted in writing and should clearly state “formal appeal request.” providers should state the specific.
The Unitedhealthcare Provider Portal Allows You To Submit Referrals, Prior Authorizations, Claims, Claim Reconsideration And Appeals,.
Appeal requests must be submitted in writing and should clearly state “formal appeal request.” providers should state the specific reason for. Complete all information required on the “request for claim review form”. To file an appeal in writing, please complete the medicare plan appeal and grievance form (pdf) (760.99 kb) and follow the instructions. Incomplete submissions will be returned.