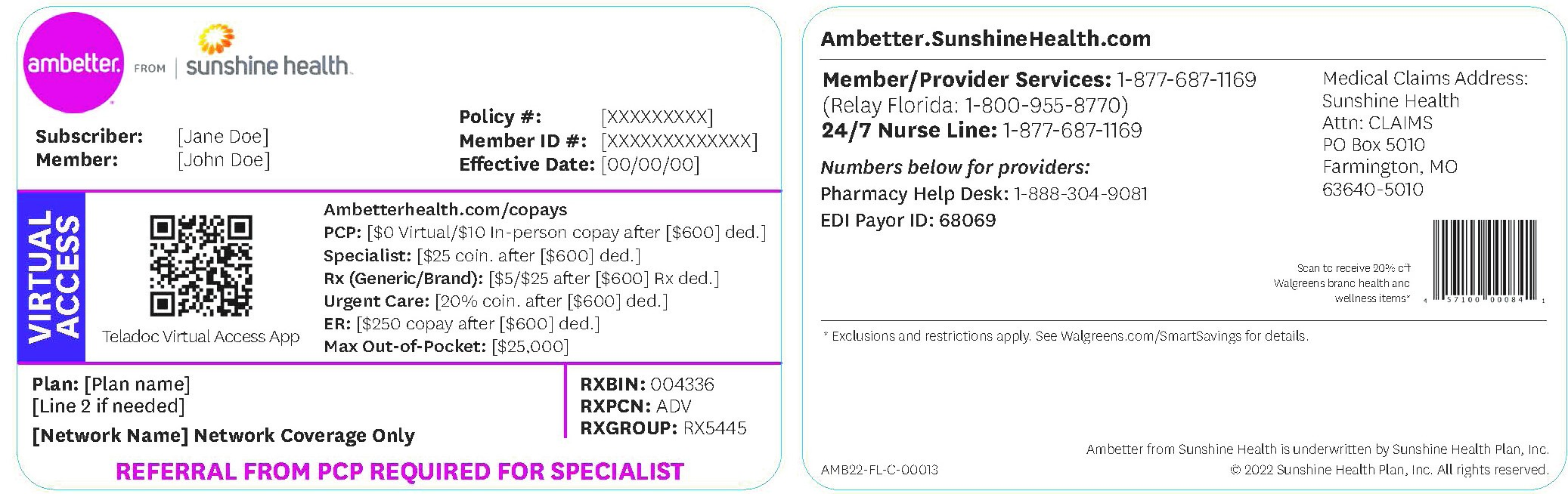
Sunshine Health Provider Appeal Form - At sunshine health, both members and providers have the right to appeal decisions that affect their care and services. Any photocopied, black & white, or handwritten claim forms, regardless of the submission type (first time, corrected claim, request for reconsideration, or claim dispute) will cause an upfront rejection. Sunshine health must resolve the standard appeal within 30 days and an expedited appeal within 48 hours. Providers may request an “expedited plan appeal” on their patients’ behalf if they believe. Use the provider claim adjustment request form to request adjustment of claim payment received that does not correspond with payment expected. Download the provider claim adjustment request form (pdf). The procedures for filing a complaint/grievance or. To ensure that ambetter member’s rights are protected, all ambetter members are entitled to a complaint/grievance and appeals process.
Download the provider claim adjustment request form (pdf). Sunshine health must resolve the standard appeal within 30 days and an expedited appeal within 48 hours. To ensure that ambetter member’s rights are protected, all ambetter members are entitled to a complaint/grievance and appeals process. Any photocopied, black & white, or handwritten claim forms, regardless of the submission type (first time, corrected claim, request for reconsideration, or claim dispute) will cause an upfront rejection. The procedures for filing a complaint/grievance or. At sunshine health, both members and providers have the right to appeal decisions that affect their care and services. Providers may request an “expedited plan appeal” on their patients’ behalf if they believe. Use the provider claim adjustment request form to request adjustment of claim payment received that does not correspond with payment expected.
Use the provider claim adjustment request form to request adjustment of claim payment received that does not correspond with payment expected. Download the provider claim adjustment request form (pdf). Sunshine health must resolve the standard appeal within 30 days and an expedited appeal within 48 hours. The procedures for filing a complaint/grievance or. To ensure that ambetter member’s rights are protected, all ambetter members are entitled to a complaint/grievance and appeals process. At sunshine health, both members and providers have the right to appeal decisions that affect their care and services. Providers may request an “expedited plan appeal” on their patients’ behalf if they believe. Any photocopied, black & white, or handwritten claim forms, regardless of the submission type (first time, corrected claim, request for reconsideration, or claim dispute) will cause an upfront rejection.
Does Sunshine Health Cover Dermatologist
To ensure that ambetter member’s rights are protected, all ambetter members are entitled to a complaint/grievance and appeals process. Use the provider claim adjustment request form to request adjustment of claim payment received that does not correspond with payment expected. Providers may request an “expedited plan appeal” on their patients’ behalf if they believe. At sunshine health, both members and.
Top United Healthcare Appeal Form Templates Free To Download In PDF
Providers may request an “expedited plan appeal” on their patients’ behalf if they believe. Any photocopied, black & white, or handwritten claim forms, regardless of the submission type (first time, corrected claim, request for reconsideration, or claim dispute) will cause an upfront rejection. Sunshine health must resolve the standard appeal within 30 days and an expedited appeal within 48 hours..
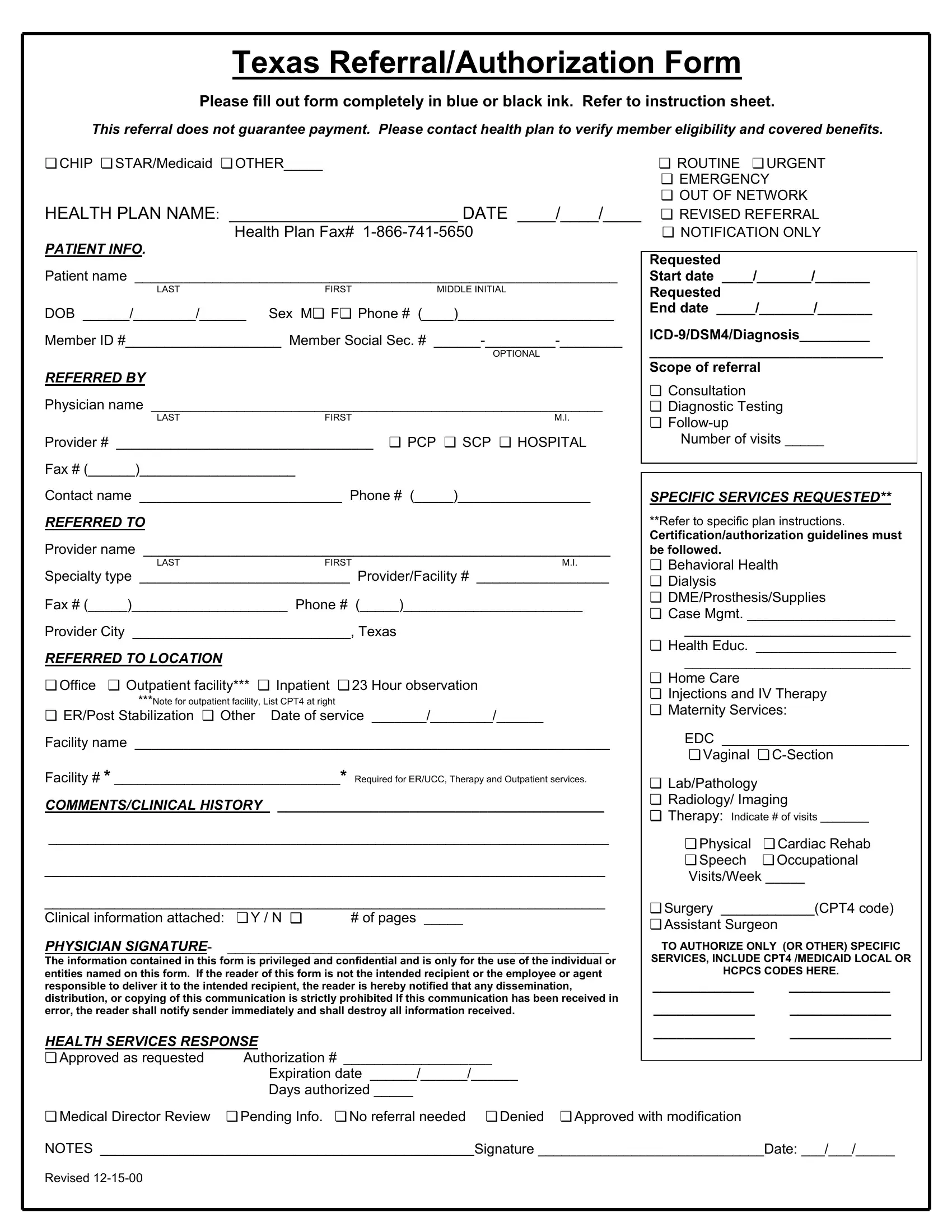
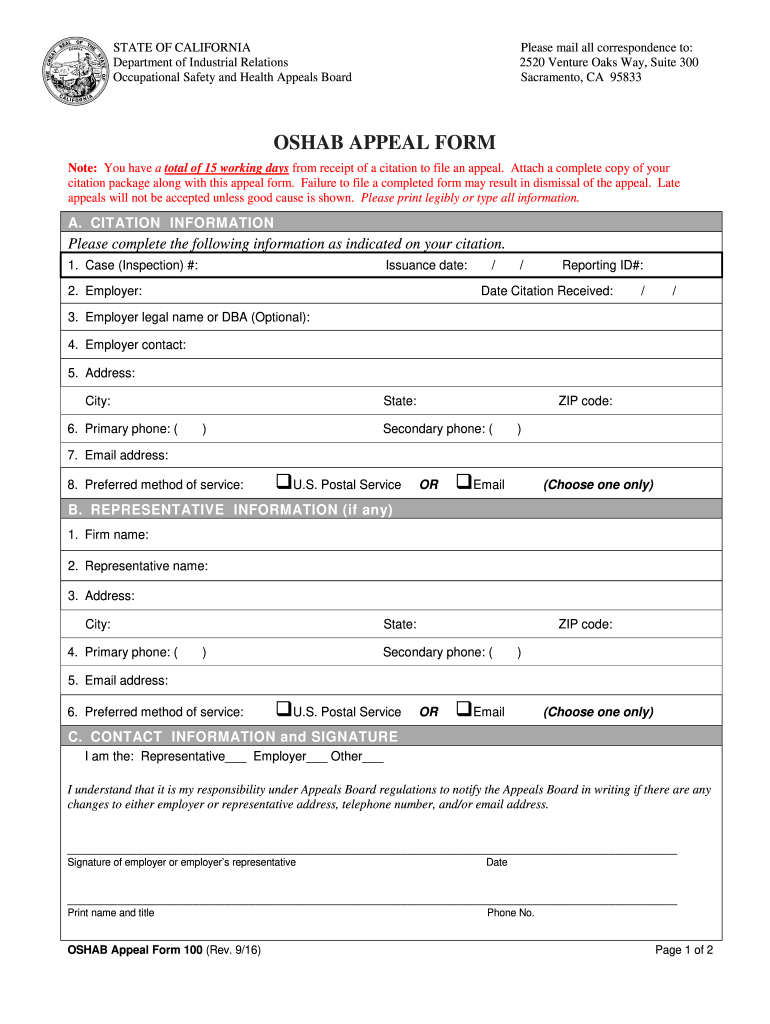
Health Plan Appeal Form ≡ Fill Out Printable PDF Forms Online
Providers may request an “expedited plan appeal” on their patients’ behalf if they believe. Use the provider claim adjustment request form to request adjustment of claim payment received that does not correspond with payment expected. Download the provider claim adjustment request form (pdf). To ensure that ambetter member’s rights are protected, all ambetter members are entitled to a complaint/grievance and.
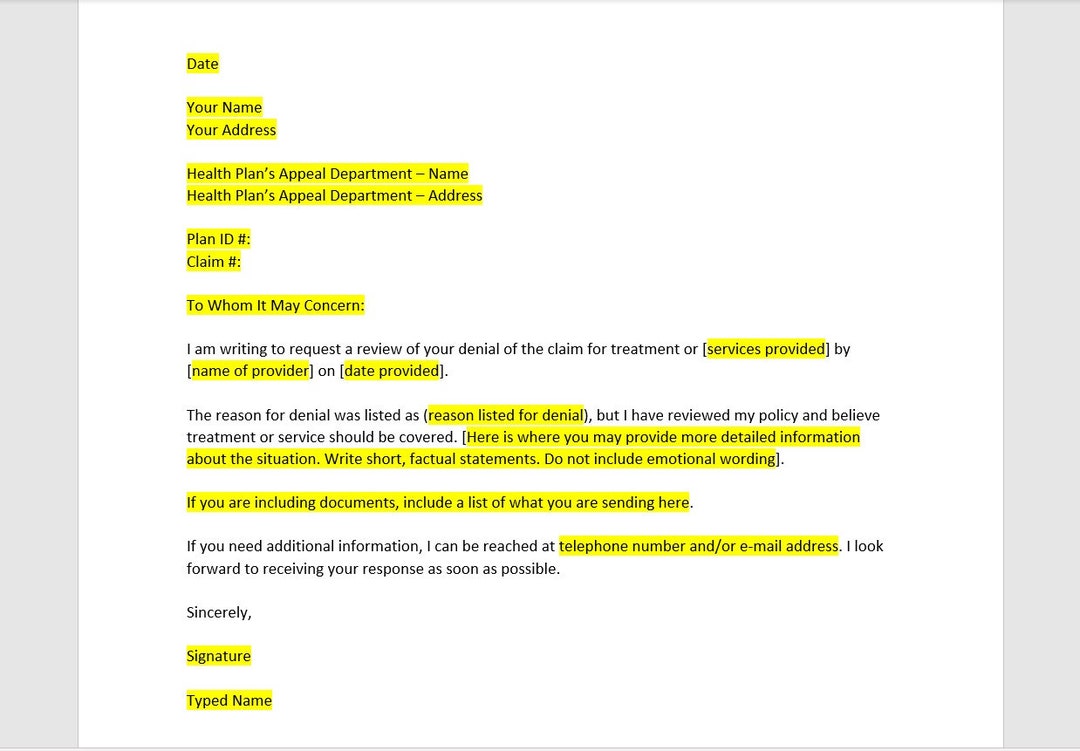
Health Insurance Appeal Letter Template, Health Insurance Appeal Letter
The procedures for filing a complaint/grievance or. Sunshine health must resolve the standard appeal within 30 days and an expedited appeal within 48 hours. At sunshine health, both members and providers have the right to appeal decisions that affect their care and services. Download the provider claim adjustment request form (pdf). Any photocopied, black & white, or handwritten claim forms,.
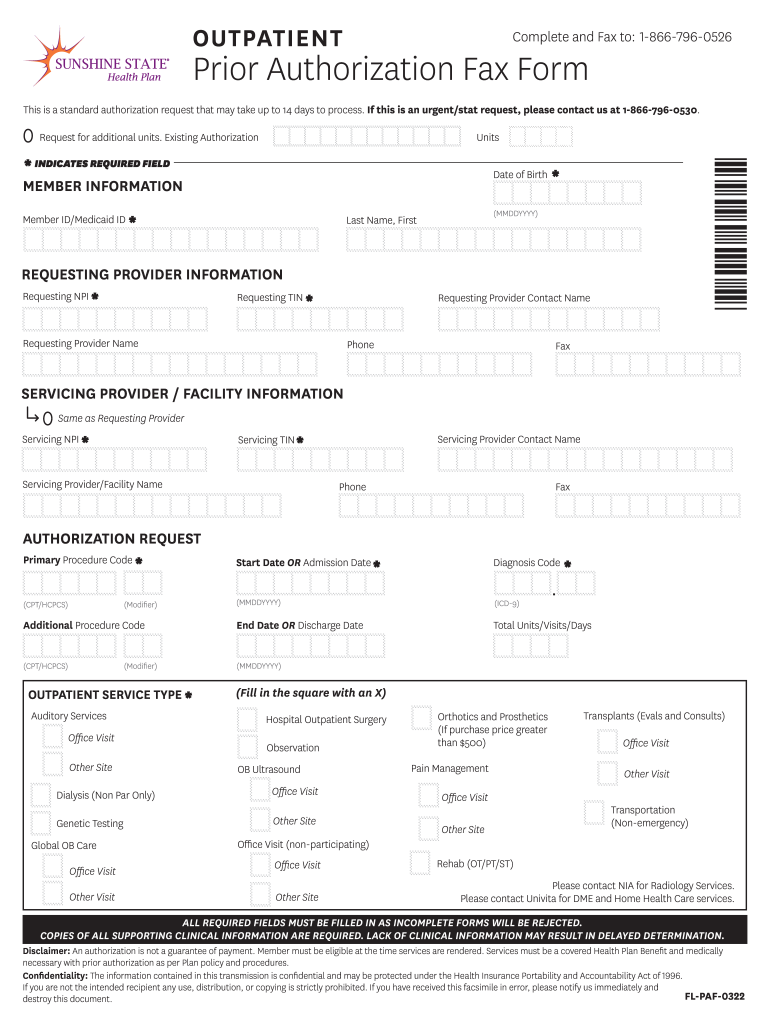
20212024 FL Sunshine State Health Plan Prior Authorization Fax Form
Use the provider claim adjustment request form to request adjustment of claim payment received that does not correspond with payment expected. Download the provider claim adjustment request form (pdf). At sunshine health, both members and providers have the right to appeal decisions that affect their care and services. To ensure that ambetter member’s rights are protected, all ambetter members are.
Sunshine Authorization Form Edit & Share airSlate SignNow
To ensure that ambetter member’s rights are protected, all ambetter members are entitled to a complaint/grievance and appeals process. Sunshine health must resolve the standard appeal within 30 days and an expedited appeal within 48 hours. Any photocopied, black & white, or handwritten claim forms, regardless of the submission type (first time, corrected claim, request for reconsideration, or claim dispute).
Erisa Appeal 20162024 Form Fill Out and Sign Printable PDF Template
Sunshine health must resolve the standard appeal within 30 days and an expedited appeal within 48 hours. Providers may request an “expedited plan appeal” on their patients’ behalf if they believe. Download the provider claim adjustment request form (pdf). Use the provider claim adjustment request form to request adjustment of claim payment received that does not correspond with payment expected..
Provider Resources, Manuals & Forms Ambetter from Sunshine Health
The procedures for filing a complaint/grievance or. Use the provider claim adjustment request form to request adjustment of claim payment received that does not correspond with payment expected. At sunshine health, both members and providers have the right to appeal decisions that affect their care and services. Providers may request an “expedited plan appeal” on their patients’ behalf if they.
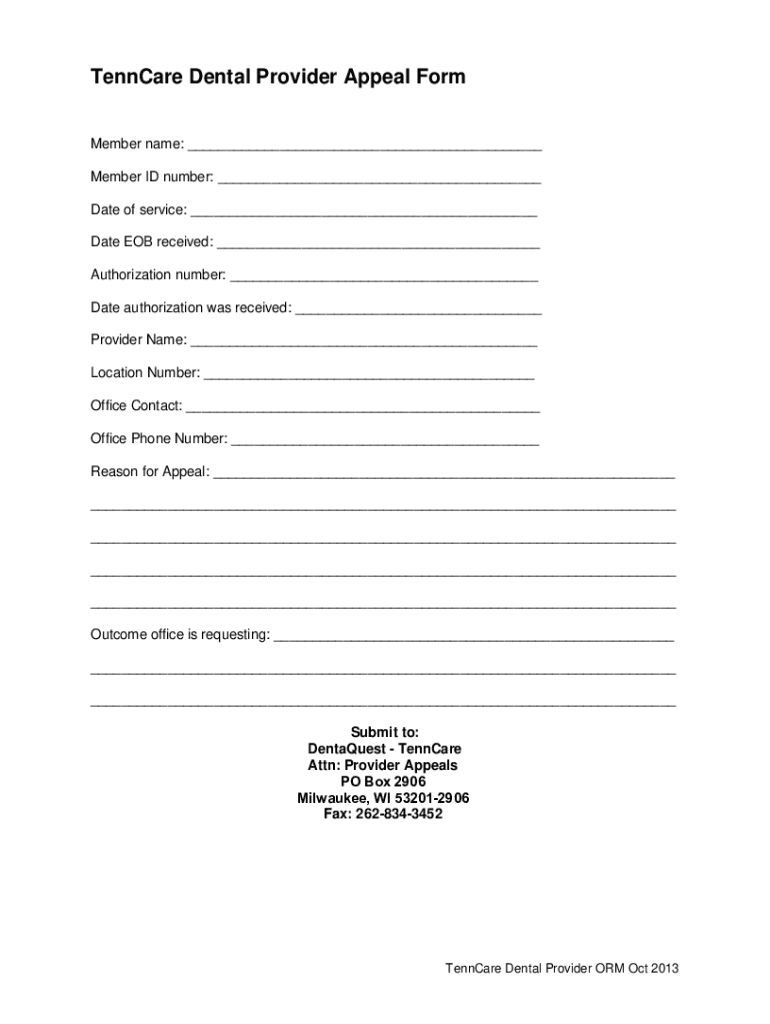
Fillable Online TennCare Dental Provider Appeal Form Fax Email Print
Download the provider claim adjustment request form (pdf). The procedures for filing a complaint/grievance or. Providers may request an “expedited plan appeal” on their patients’ behalf if they believe. Use the provider claim adjustment request form to request adjustment of claim payment received that does not correspond with payment expected. Any photocopied, black & white, or handwritten claim forms, regardless.
Fill Free fillable Sunshine Health PDF forms
The procedures for filing a complaint/grievance or. Use the provider claim adjustment request form to request adjustment of claim payment received that does not correspond with payment expected. Download the provider claim adjustment request form (pdf). Any photocopied, black & white, or handwritten claim forms, regardless of the submission type (first time, corrected claim, request for reconsideration, or claim dispute).
Download The Provider Claim Adjustment Request Form (Pdf).
Any photocopied, black & white, or handwritten claim forms, regardless of the submission type (first time, corrected claim, request for reconsideration, or claim dispute) will cause an upfront rejection. Sunshine health must resolve the standard appeal within 30 days and an expedited appeal within 48 hours. The procedures for filing a complaint/grievance or. To ensure that ambetter member’s rights are protected, all ambetter members are entitled to a complaint/grievance and appeals process.
At Sunshine Health, Both Members And Providers Have The Right To Appeal Decisions That Affect Their Care And Services.
Use the provider claim adjustment request form to request adjustment of claim payment received that does not correspond with payment expected. Providers may request an “expedited plan appeal” on their patients’ behalf if they believe.