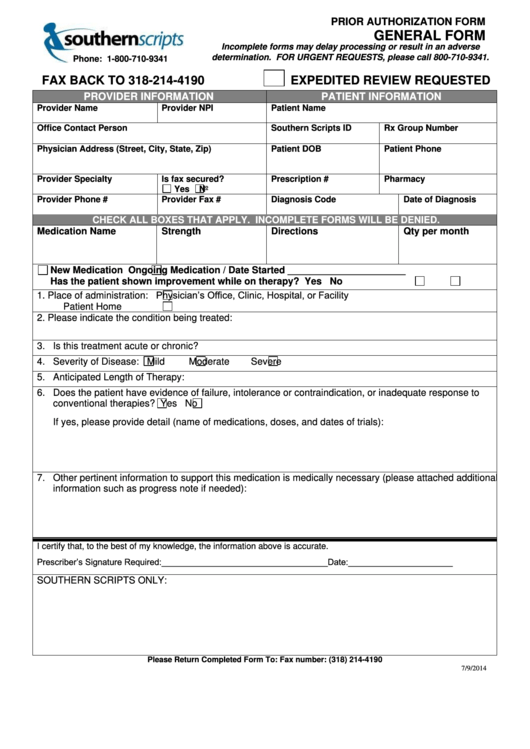
Southern Scripts Prior Authorization Form - To file an appeal for denied benefit coverage, complete this form and return to liviniti with clinical documentation. Before you get started, in addition to your insurance card, you will need the following information. This information can be obtained. To perform a prior authorization drug lookup, use the interactive formulary search found on your member page. Submit a prior authorization request or appeal using the links below. Submit a prior authorization request. Visit our pharmacy portal for pricing or appeal information.
Before you get started, in addition to your insurance card, you will need the following information. To perform a prior authorization drug lookup, use the interactive formulary search found on your member page. This information can be obtained. Submit a prior authorization request or appeal using the links below. Submit a prior authorization request. Visit our pharmacy portal for pricing or appeal information. To file an appeal for denied benefit coverage, complete this form and return to liviniti with clinical documentation.
Submit a prior authorization request or appeal using the links below. This information can be obtained. Submit a prior authorization request. Visit our pharmacy portal for pricing or appeal information. To perform a prior authorization drug lookup, use the interactive formulary search found on your member page. To file an appeal for denied benefit coverage, complete this form and return to liviniti with clinical documentation. Before you get started, in addition to your insurance card, you will need the following information.
Fillable Online Southern scripts prior authorization form pdf. Southern
This information can be obtained. Submit a prior authorization request or appeal using the links below. Visit our pharmacy portal for pricing or appeal information. Before you get started, in addition to your insurance card, you will need the following information. To perform a prior authorization drug lookup, use the interactive formulary search found on your member page.
First Script Prior Authorization Form
To perform a prior authorization drug lookup, use the interactive formulary search found on your member page. To file an appeal for denied benefit coverage, complete this form and return to liviniti with clinical documentation. Submit a prior authorization request. This information can be obtained. Visit our pharmacy portal for pricing or appeal information.
Fillable Prior Authorization Form Southern Scripts printable pdf download
This information can be obtained. Submit a prior authorization request or appeal using the links below. Before you get started, in addition to your insurance card, you will need the following information. To perform a prior authorization drug lookup, use the interactive formulary search found on your member page. Submit a prior authorization request.
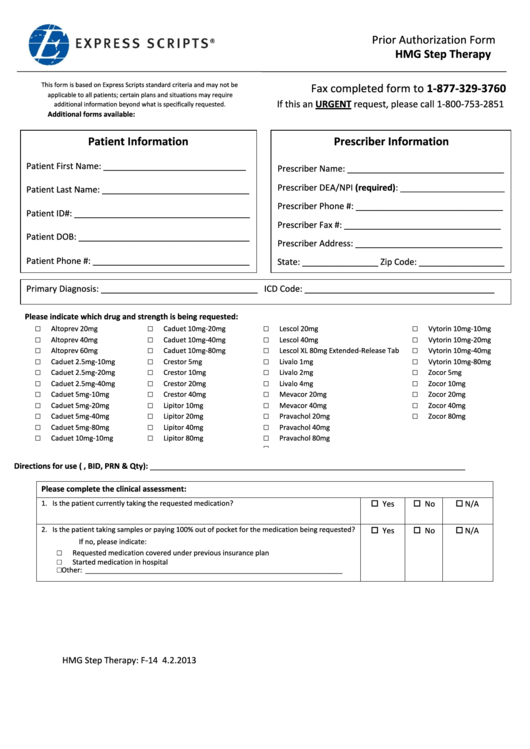
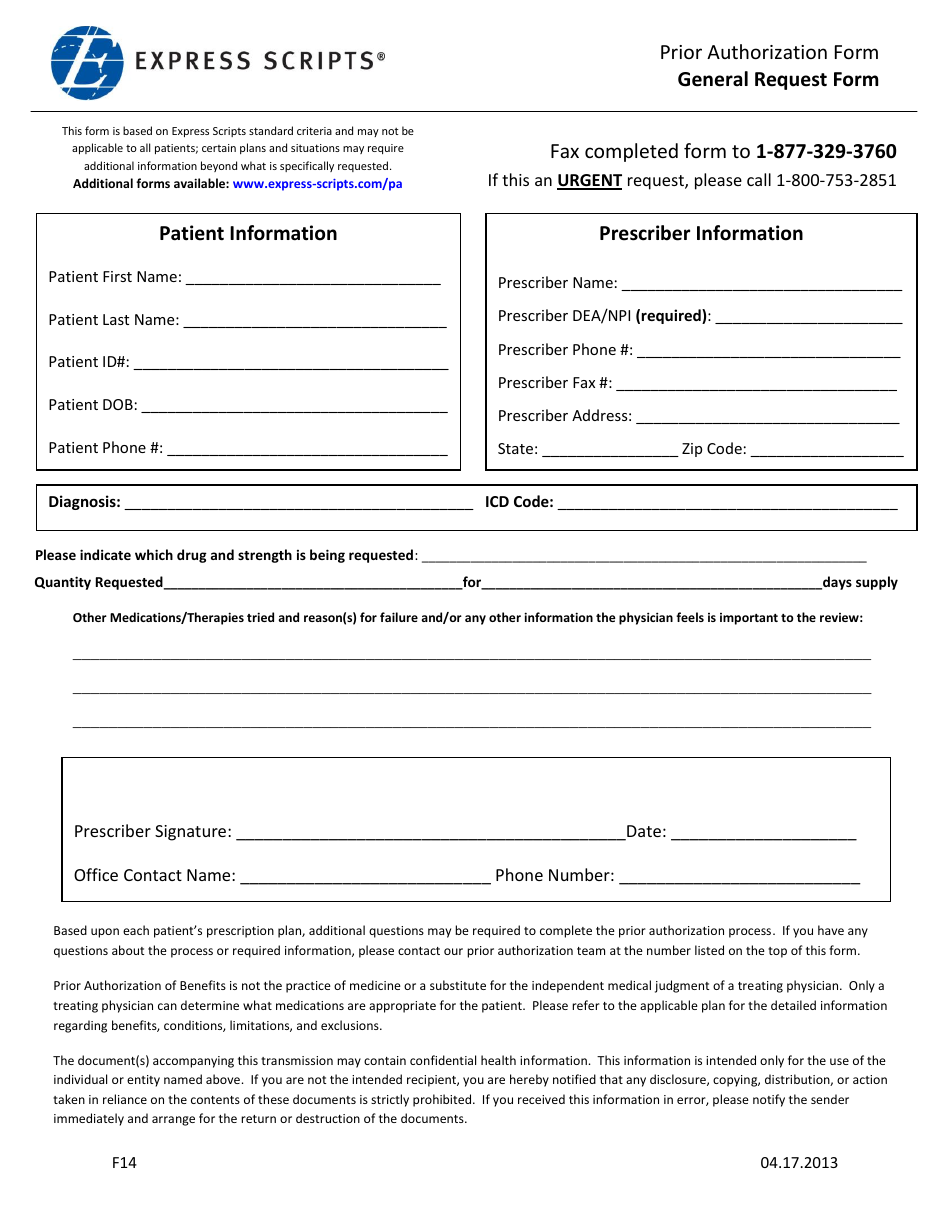
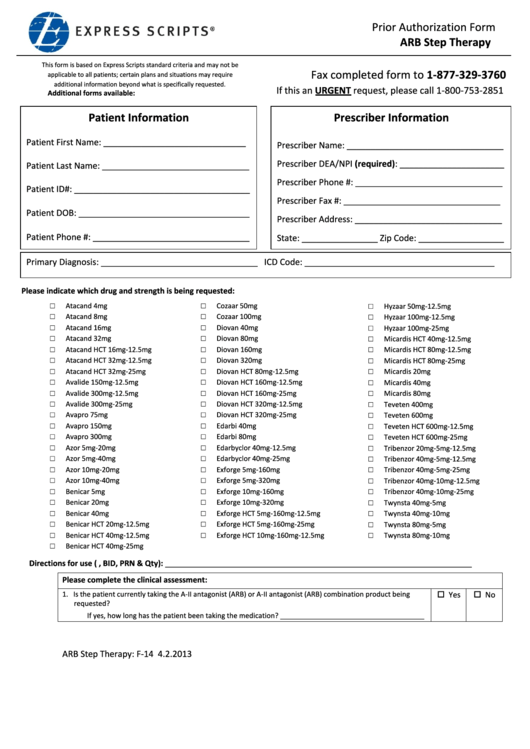
Express Scripts Prior Authorization Form Pdf
To perform a prior authorization drug lookup, use the interactive formulary search found on your member page. Submit a prior authorization request. This information can be obtained. Before you get started, in addition to your insurance card, you will need the following information. Submit a prior authorization request or appeal using the links below.
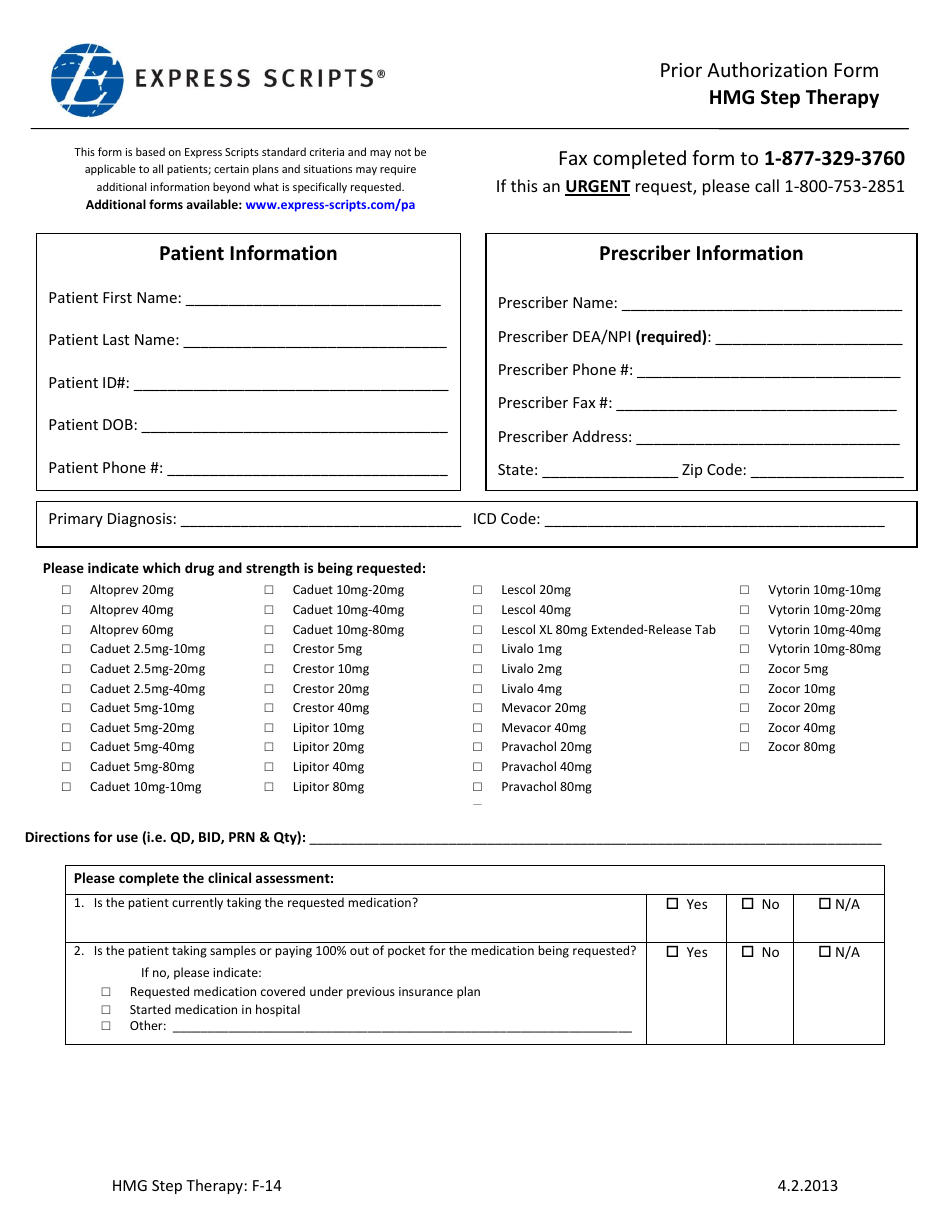
Express Scripts Prior Authorization Form Hmg Step Therapy printable
To file an appeal for denied benefit coverage, complete this form and return to liviniti with clinical documentation. Submit a prior authorization request or appeal using the links below. Submit a prior authorization request. Visit our pharmacy portal for pricing or appeal information. Before you get started, in addition to your insurance card, you will need the following information.
Form F14 Fill Out, Sign Online and Download Fillable PDF Templateroller
Submit a prior authorization request or appeal using the links below. To perform a prior authorization drug lookup, use the interactive formulary search found on your member page. This information can be obtained. To file an appeal for denied benefit coverage, complete this form and return to liviniti with clinical documentation. Before you get started, in addition to your insurance.
Form F14 Fill Out, Sign Online and Download Printable PDF
This information can be obtained. To file an appeal for denied benefit coverage, complete this form and return to liviniti with clinical documentation. Submit a prior authorization request or appeal using the links below. Submit a prior authorization request. To perform a prior authorization drug lookup, use the interactive formulary search found on your member page.
Express Scripts Prior Authorization Form Arb Step Therapy printable
This information can be obtained. Visit our pharmacy portal for pricing or appeal information. To perform a prior authorization drug lookup, use the interactive formulary search found on your member page. Submit a prior authorization request or appeal using the links below. Before you get started, in addition to your insurance card, you will need the following information.
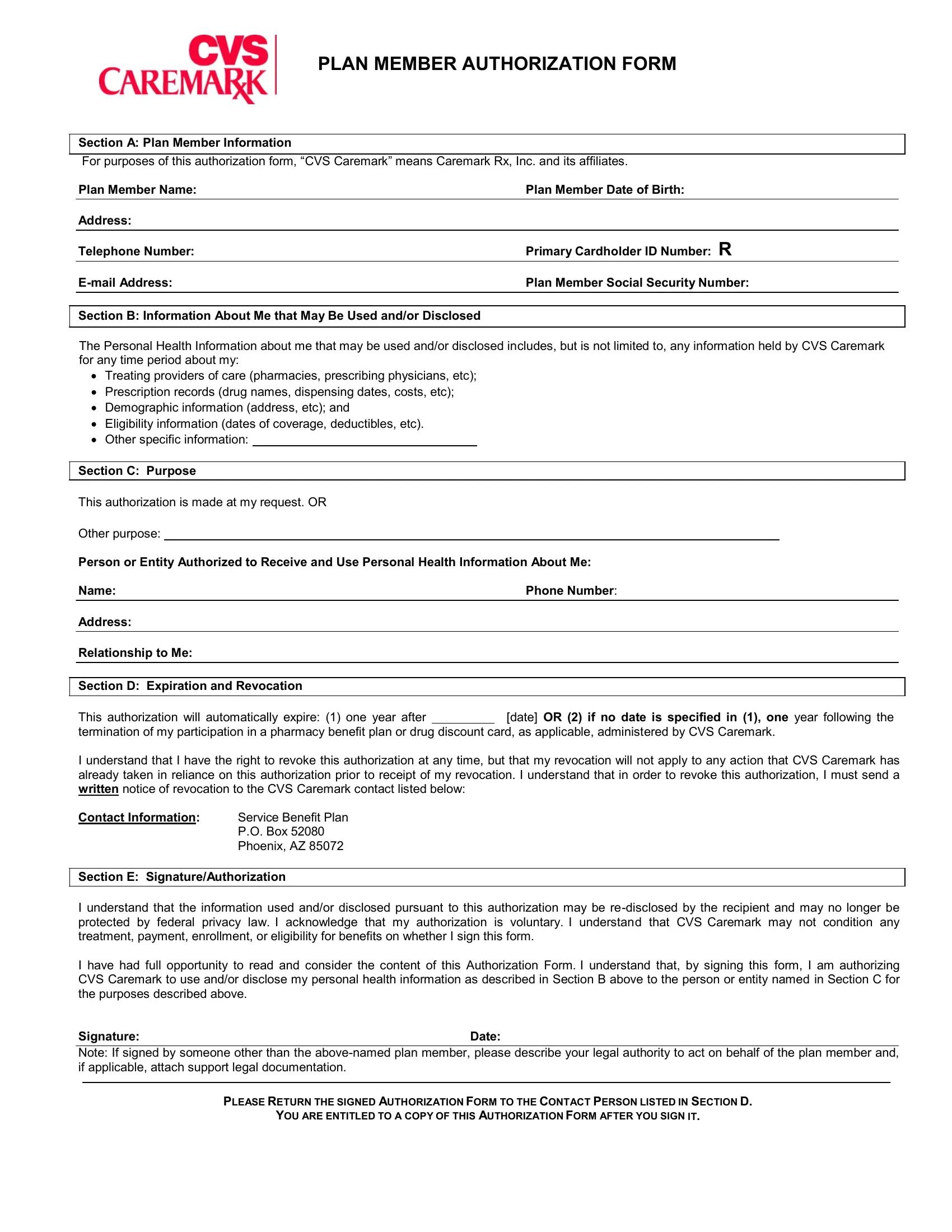
Member Authorization Form ≡ Fill Out Printable PDF Forms Online
Submit a prior authorization request or appeal using the links below. Visit our pharmacy portal for pricing or appeal information. This information can be obtained. To perform a prior authorization drug lookup, use the interactive formulary search found on your member page. Submit a prior authorization request.
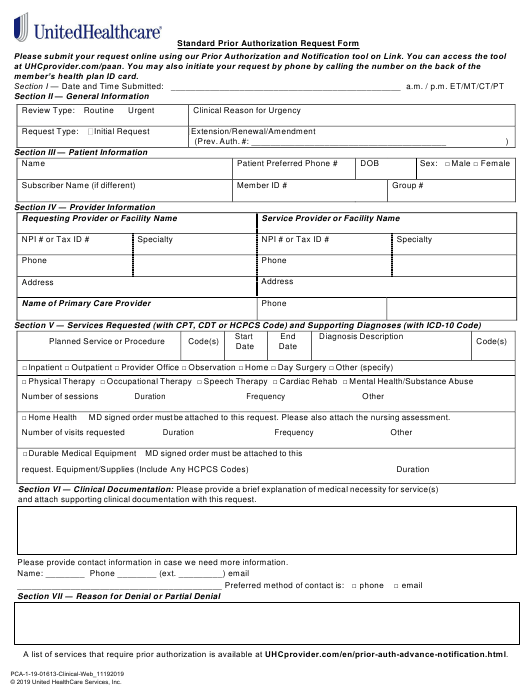
Unitedhealthcare Community Plan Prior Authorization Form Washington
Visit our pharmacy portal for pricing or appeal information. This information can be obtained. Submit a prior authorization request or appeal using the links below. Submit a prior authorization request. Before you get started, in addition to your insurance card, you will need the following information.
To Perform A Prior Authorization Drug Lookup, Use The Interactive Formulary Search Found On Your Member Page.
Visit our pharmacy portal for pricing or appeal information. Before you get started, in addition to your insurance card, you will need the following information. Submit a prior authorization request or appeal using the links below. Submit a prior authorization request.
To File An Appeal For Denied Benefit Coverage, Complete This Form And Return To Liviniti With Clinical Documentation.
This information can be obtained.